Discharge and admission avoidance – system resources
Welcome to the Discharge Resources Page for health and care professionals in the Manchester and Trafford system
This page is designed to provide health and care professionals in the Manchester and Trafford system with useful resources to support effective discharge of patients from hospital and admission avoidance.
You can find information on a wide range of discharge and admission avoidance related topics in the drop down menus below. If there are other resources that would be useful to have on this page please let us know by emailing communications@manchesterlco.org
Discharge resources and information
Use the drop downs below to access useful information on each topic.
The Alternatives to Admission Guides are a regularly updated single page handy guide to core services that primary care and hospital staff can use to direct patients to other services. Includes contacts for community response services, Hospital at Home, mental health, eye care and VCSE sector. There are guides for each locality:
- North Manchester (NMGH) Alternatives to Admission Dec 2024 [PDF]
- Central Manchester (MRI) Alternatives to Admission Dec 2024 [PDF]
- South Manchester (Wythenshawe) Alternatives to Admission Dec 2024 [PDF]
- Trafford Alternatives to Admission Dec 2024 [PDF].
If you find any incorrect information at all in these guides please contact communications@manchesterlco.org
Home First is the Manchester and Trafford Local Care Organisations and system partners’ approach to hospital discharge improvement.
A key part of our role in the LCO is to avoid people going in to hospital. If they do need hospital care for a period of time then we work with the hospitals to get them home or back in the community as soon as possible.
We have several approaches to support this work. This includes establishing Manchester and Trafford centralised discharge control rooms which coordinate all hospital discharges. Health and social care staff work together in the control rooms to expedite discharges and solve problems that may delay a patient’s discharge.
A range of other work has been carried out as part of what we called the Resilient Discharge Programme – developing strengths based approaches to discharge.
- You can find a range of Home First Resources on this page including our Resource Guide and staff video
- These are also available on the MFT staff intranet/extranet (look under hospitals/MCS in the LCO section).
Home First video
All hospital staff are encouraged to watch the Home First at MFT video (10 mins) that provides an overview of the Home First approach and useful information and case studies on how to plan for discharge.
Home First back to basics discharge resource guide
The Home First resource guide is an informative training booklet for ward staff. It includes practical steps and advice on strengths-based discharge, guides to pathways, community services and much more. It is based on real work in the hospitals to improve discharge processes.
- Home First Resource Guide [PDF, 770KB]
Other useful resources
Discharge to Access (D2A) Pathways [PPT, 93KB]
National Discharge Leaflets [Word doc, 115KB]
Hospital at Home is a new model of care in the NHS that provides the acute level care and monitoring that patients expect in a hospital, delivered in the place they call home. It combines the community and acute offers in services in each locality of Manchester. These services are now live and open to referrals from hospital teams (step down from hospital) and primary care (step up from community).
Our service pages have more information on the live offers, the team of staff who provide the service and referral information for healthcare professionals.
What is Home from Hospital?
Home from Hospital is a voluntary sector service that supports patients leaving hospital who need that extra bit of support to settle back at home. Many patients may have struggled at home prior to admission. Typical issues include homes being unheated, not having utility funding, no food in the property and basic adaptations. Home from Hospital responds to these kind of needs and resettles patients back home with enough support for up to 4 weeks. They provide regular face to face contact and telephone support to respond to issues quickly. Services also include transport on discharge, pet care and more.
Providers and referral contacts
There are 3 providers of Home from Hospital services across MFT for residents of Manchester:
- Manchester Care and Repair (North Manchester General Hospital – all pathways supported)
- Age UK Manchester (MRI and Wythenshawe Hospital – all pathways supported)
- Royal Voluntary Service (MRI only – pathway 0 supported only).
Full information of what is available on each site – including referral contacts and provision available – here:
Home from Hospital Winter 2023 [PDF, 381KB]
Technology enabled care (known as TEC or technology enabled care services) refers to a number of devices and apps that people can use to help them stay safe and independent at home, at work or within their local community. They are provided by Manchester City Council’s Community Alarms and Technology Enabled Care Team (CATEC) which is part of Manchester Local Care Organisation.
TEC is a key part of our strategy to keep people independent as possible in the community. It can also help reduce the amount of face-to-face care someone needs while providing the reassurance to families and carers that they are safe.
You can download our new Technology Enabled Care brochure with all the items we offer here – Technology Enabled Care Brochure [PDF]
There is a range of technology available and what would be best for you depends on your circumstances. You can see them all in the brochure, however, our most popular options are:
Community alarm
This is a base unit that connects to a small device that can be worn discreetly around your wrist or neck. It can send alerts or call carers, family or the CATEC team if you need help in your own home. A community alarm can also link to other devices, such as a smoke alarm.
This is often used by people who are at risk of falls at home.
A black and white drawing of a community alarm device
GPS device
A GPS device can be moved around and gives real-time location information. This means that if you get lost, you can be found by carers, family or the CATEC team.
This is often used by people with memory issues who would like to remain independent in their own home without worrying about getting lost.
A black and white drawing of a GPS tracker
Household sensors
Household sensors can detect a variety of things, including movement, epileptic seizures, incontinence, floods, carbon monoxide and open doors. Sensors can automatically turn on lights to reduce the risk of falls and send alerts if you need support.
Household sensors also include JustChecking – a simple web-based activity monitoring system, using wireless sensors in the home to generate an activity chart, which can be used to support future decision making to promote independence.
Household sensors are often used by people who would like to remain independent but who need peace of mind for themselves and their loved ones.
A black and white drawing of a household sensor
YOURmeds
YOURmeds is a portable medication dispenser that provides you with timed visual and audible reminders to take your medication. If a medication dose is missed, an alert is sent so you can be supported.
This is often used by people who sometimes forget to take their medication at the correct time.
An image of the medication weekly pill organiser
What are the benefits of technology enabled care?
Our simple and easy-to-use devices can be useful for a range of situations. They offer several benefits such as:
- They allow you to maintain your independence and keep you safe, alerting your carers, family or CATEC team when you need support.
- They give your loved one’s peace of mind, as they know you are safe.
- They are inexpensive. Monitoring costs for community alarms start from £4.10 per week. The devices themselves are free.
- They are easy to use and discreet.
Watch and listen to this video of David whose father Harry lives with Dementia. David explains how technology enabled care has helped Harry stay in his own home and out of hospital.
Referral process and contact information
For some of our devices you can self-refer. However, for others such as the GPS device, a referral from a health or social care professional is required. By health and care professional we mean a nurse, doctor (GP or consultant) or a social worker.
If you are interested in a TEC device, please contact the Manchester City Council Contact Centre on 0161 234 5001 or email at mcsreply@manchester.gov.uk
CATEC Team opening hours
The CATEC operate 24 hours a day, 365 days a year. They install, monitor and respond to devices.
Downloads
Video Guides
Use the below videos to help you learn more about the technology enabled care devices we have available. Craig from the CATEC explains the benefits and how they work.
- Door sensors
Video with captions
Video without captions
- Chair, bed and pressure mat sensors
Video with captions
Video without captions
- Epilepsy sensor
Video with captions
Video without captions
- GPS tracker with SOS button, falls detection and tracking device
Video with captions
Video without captions
- Falls Detector
Video with captions
Video without captions
Full playlist of Video Guides available here.
The service provides ‘one off’ cleaning in domestic properties that do not meet acceptable health and safety standards. Referrers do need to consider what ongoing support someone may need in managing their hoarding behaviours. Where a property is extremely cluttered due to a long period of hoarding, referrers need to consider if Crisis Clean is right service to support that citizen.
Crisis Clean Criteria Full Information [Word doc, 37KB]
MCC Adult Social Care Crisis Clean [PPT, 127KB]
Contents
- Crisis Clean Service Criteria
- Crisis Clean Service Specification
- Consent
- Access to Properties
- Funding
- Crisis Clean Service Criteria
In order to access the Crisis Clean Service citizens must meet the following criteria
- Must be over 18 years old
- Must reside in the City of Manchester. The service does not cover other Greater Manchester boroughs
- Must be intending to reside in the property for at least a further 6 months at the time of the referral
- Must be able to give consent or have an advocate or Power of Attorney who can give consent on their behalf
- Crisis Clean Service Specification
The service provides ‘one off’ cleaning in domestic properties that do not meet acceptable health and safety standards. This includes
- Where an individual is at risk due to the environmental conditions they are living in
- To enable a person to return home to a safe environment; from hospital, residential care or staying with family or friends.
- When health and social care staff or other professionals are unable to go in to provide a service on health and safety grounds.
- Where an individual’s tenancy is ‘at risk’ due to the environmental condition of the property.
Where a property is extremely cluttered due to a long period of hoarding, referrers need to consider if Crisis Clean is right service to support that citizen. Crisis Clean is a ‘one off’ service so referrers do need to consider what ongoing support someone may need in managing their hoarding behaviours.
Crisis Clean will support citizens who hoard but referrers need to be realistic about what can be achieved in a short period of time and be specific about what tasks and outcomes they want from the clean.
If the job will take more than 2 shifts it is too big for us to take on.
Tasks that the Crisis Clean service can support with:
Any tasks that Crisis Clean are to undertake must be specified on the referral form and agreed prior to the clean commencing. This includes:
- General/ deep household cleaning of kitchens, bathrooms, bedrooms and reception rooms
- Removal of unwanted clutter and smaller furniture items, within reason.
Tasks that the Crisis Clean service does NOT support with:
- Any type of decoration, DIY or home improvements
- Clearing of garden areas or garden rubbish
- Removal of large items of furniture or carpets
- Change curtains, wash windows or do any type of laundry
- Defrost fridges or freezers
- Dispose of out-of-date medication
- Full house clearances
- Clearance of individual rooms that are not in use, and do not affect the safety of staff/citizen.
- Consent
The Crisis Clean service needs to have written agreement to work in citizen’s properties.
Wherever possible this should come from the citizen themselves.
If this is not possible, this must come from someone acting on their behalf. This may be an agreed friend or family member, or it could be someone professionally involved, acting as their advocate.
The Crisis Clean service will normally only dispose of unwanted items when the citizen or their advocate is present to agree what is being removed.
If it is not possible for the citizen or their advocate to be present at the time of the clean, staff will only dispose of items where specific written permission has been given to do this.
- Access to Properties
It is preferable that either the citizen or their advocate is present in the property while the clean takes place.
If this is not possible, it is up to the referrer to arrange access for the Crisis Clean workers.
The Crisis Clean service do not hold, drop off or pick up keys. Referrers can drop off keys at the Crisis Clean office before 9.00am on the day of the clean but must ensure they pick them up before 4.30pm on the same day as there is no secure storage facilities for keys. This must be agreed prior to the day of the clean.
In the case where Crisis Clean workers cannot again access to a property on the agreed day, the referral will be cancelled.
In the case where Crisis Clean workers cannot gain access to a property on the agreed day, for services where charges apply (see section 5: Funding and Costs) a charge of one hour will still apply plus the cost of any skip hire.
- Funding and Costs
The Crisis Clean service is funded by Manchester City Council’s Adult Services Division. Due to this there is no additional charge for referrals from teams that sit within this Division.
For referrals from any other services the following charges apply:
Hourly Rate: £45
Skip Hire (if required) £290
No Access Charge: £45 plus any skip hire cost
Funding must be agreed /approved by the budget holder prior to the clean taking place.
Invoices will be issued via SAP once the clean has been completed.
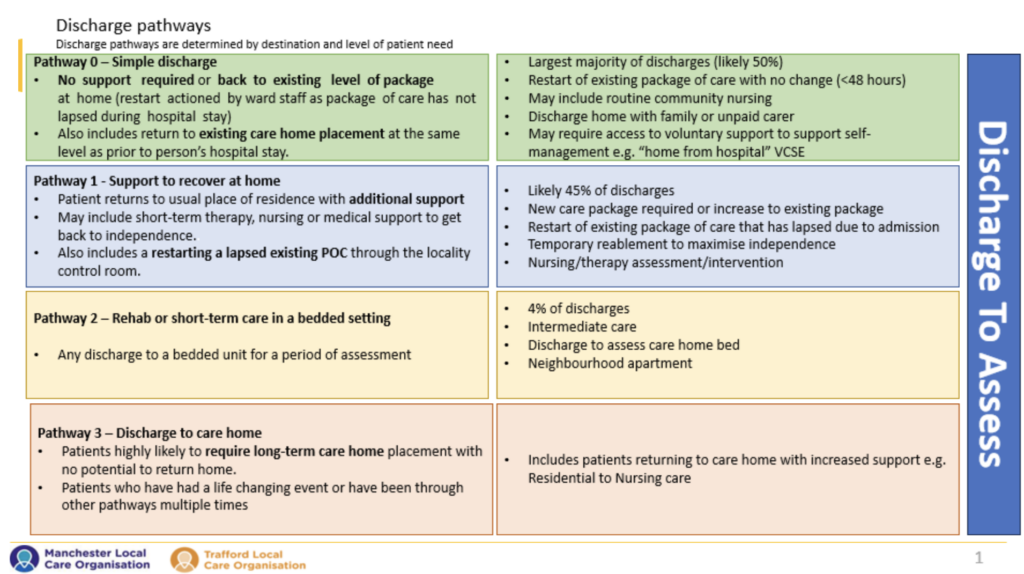
Pathway 0 – Simple discharge home/to usual place of residence coordinated by the ward
- no new or additional health and/or social care and support
- self-management with signposting to services in the community
- voluntary sector support
- re-start of pre-existing home care package at the same level without involvement of the transfer of care hub
- returning to original care home placement with care at the same level as prior to the person’s hospital stay.
Pathway 1 – Support to recover at home
Pathway 1 is for people discharged home (to their usual place of residence or temporary accommodation) with support co-ordinated by the Care Transfer Hub (Integrated Discharge Team, Control room and Brokerage). This might include short-term therapy, nursing or medical support to get back to independence. For those with less rehab potential, P1 is also used to trial a package of care in the short-term to assess longer-term needs.
-
Re-start of home care package at the same level as a pre-existing package that lapsed in the community
-
A new home care package in the community
-
Long-term care home care package and support at home following a period of intermediate care or reablement in the community
-
Reablement intervention to maximise independence
-
Short-term therapy, nursing or medical support to get back to independence
Pathway 2 – Rehab or short-term care in a bedded setting
Pathway 2 (P2) is for people who need a period of rehab in a bed based service. Bedded care is only for people who are not safe between care visits in the community. Some people will go to a rehab community bed to recover, reable and rehabilitate. Others might go to an interim bed while home care is sourced, a social issue is resolved, or to assess whether they need a long-term bed.
- Patients transferred to a non-acute bed for a period of rehabilitation before returning home.
- 4% of discharges
- Short-term rehabilitation to maximise potential.
- Bedded assessment for health and/or care needs to return home.
Referral to be completed on a Greater Manchester Supported discharge form by therapy staff with input from wider MDT as required and send to the relevant hospital single point of access email.
Manchester Intermediate care offer is a city wider offer, although control room team will attempt to place a patient if they have a preference this is often not possible.
November 2024 update – As part of the Home First Programme we are focussing on developing the Manchester community bedded care offer to align better with the national definitions, which will include a wider scope of definition for Pathway 2 beyond rehabilitation only. This will include aspects of the current Pathway 3 cohort of referrals moving to Pathway 2. At present some Pathway 3 referrals are reclassified on Hive EPR at point of discharge for data purposes, but we will look to reflect this at an earlier stage at point of referral. This page will be updated in due course to reflect these changes as they are confirmed.
In Manchester the units include:
Crumpsall Vale
North Manchester General Hospital
Delaunays Road
Crumpsall
Manchester
M8 5RB
Buccleuch Lodge Intermediate Care
Elizabeth Slinger Road
Manchester
M20 2XA
Central Manchester Intermediate Care
Delamere Unit
Gorton Parks
121 Taylor Street
Gorton
M18 8DF
For Trafford residents Pathway 2 bedded rehab is provided at
Ascot House
Ascot Avenue
Sale
M33 4GT
Above information available to download here:
Pathway 2 [Word doc, 25KB]
Pathway 3 – People discharged to long-term bed-based care.
Pathway 3 (P3) is often for people who have had a life changing event, have been through other pathways multiple times or are approaching the end of their life and may sadly be likely to quickly decline.
- Pathway 3 is a discharge to a care home for patients who are likely to require long-term bed-based care.
- Patients who have had a life changing event or have been through other pathways multiple times.
Process
- Once the pathway has been identified by the MDT, a member of the hospital integrated discharge team will lead on the completion of the referral utilising the Greater Manchester Supported Discharge Form
- Input may be required from extended members of the MDT to support the assessment and/or Mental capacity if required
- Once complete the referral is sent to the relevant local authority who will lead on the sourcing of a pathway 3 placement
- Referrals should be sent to the relevant hospitals’ single point of access email address.
North Manchester General Hospital – noticetoassess@manchester.gov.uk
Manchester Royal Infirmary- LL.discharge2assessMRI@mft.nhs.uk
WTWA – wythenshawecontactofficer@mft.nhs.uk
Key communication points to consider prior to completion of a pathway 3 referral.
The basic for good practise is to involve patients and their representatives in discharge planning from the earliest opportunity. By keeping them informed throughout the discharge journey and confidently explaining the discharge to assess process further choice issues can be avoided.
- All relevant discharge information leaflets should be provided to patients and their representatives at the earliest opportunity, leaflets form a part of the communication but do not replace regular effective, transparent engage with patients from all members of the MDT.
- A pathway 3 bed is for patients who are likely to require long-term bed-based care who have had a life changing event or have been through other pathways multiple times. It is a temporary move to a discharge to assess bed, based in a care home for a period of up to 28 days, this will likely be one of our contracted D2A beds
- The choice that patients have is to opt out of D2A, if they opt in then this means they agree that the first appropriate placement found will be accepted
- During this time, they will be visited by health and social care workers who will assess them to decide what care they need long-term you will be allocated a social worker within 48 hours of discharge to progress from the temporary plan to a long-term plan
- The temporary bed will be at the first home that has availability and is able to manage the assessed needs, this may be out of the local areas if there are limited beds that can meet specific needs
- Staying in hospital to find a home of choice is not an option because beds in the acute hospital are needed for people who are acutely unwell and the longer you stay in hospital the greater the risk of hospital acquired infections and general deconditioning
- Once they are in a D2A bed the team will work with the patient and family to find a long-term care home which they will be able to choose that suits all the needs
- The D2A bed will be paid for by the local authority until all the long-term assessments are completed (usually less than 28 days)
- Local authorities will try and place in home CQC rated as good – however there are occasions where a home rated as requires improvement may be considered if the local authority is assured through due diligence/improvement work undertaken that the home is suitable.
Above information available to download here:
Pathway 3 [Word doc, 25KB]
Manchester Community Response and Trafford Community Response
There are a number of community services in Manchester and Trafford that can support admission avoidance and effective discharge provided by the Local Care Organisations and their partners. This includes Community Response services that deliver Crisis Response and Discharge to Assess services. Trafford has launched Crisis Response and Discharge to Assess teams recently in time for Winter.
You can find flowcharts with referral information for these services here:
Manchester Community Response (MCR) Hospital Discharge Pathways [PPT, 90KB]
Trafford Community Response (TCR) flowchart [PPT, 86KB]
Service information on community services
All LCO community services including crisis response and Hospital at Home have pages with referral information on the LCO websites. You can find them here:
Community Care Navigators for Manchester and Trafford
Care Navigators are an LCO service that work across the city and borough’s hospitals and in the neighbourhoods of Manchester and Trafford. They an work with Do you know someone who you identify is:
- Socially isolated or lonely
- At risk of hospital re-admission
- Causing you worry
- Poorly connected in their community/neighbourhood
- Suitable for non-clinical intervention
- A resident or GP patient of Manchester or Trafford over 18 years old.
Care Navigators work with people to ensure they are connected with the right services available to them in your local neighbourhood. They work closely with other NHS services, mental health services, GP’s, social services (council), housing associations, charities, voluntary groups, social enterprise organisations and other community resources to do this.
If you would like to talk to a Care Navigator or make a referral, please contact the Single Point of Access (SPA) team by phone or email:
Tel: 0300 303 9650
E-mail: mft.spa-uhsm@nhs.net
Hive is the MFT electronic patient record system and has brought a range of functionality to support effective discharge. This includes Board Round functions that can support effective discharge planning.
All information can be found on the HIVE MFT intranet page here.
Discharge for patients with palliative and end of life care needs
Discharge planning for patients with palliative and end of life care needs can be complex. Additional measures should be taken to ensure all aspects of care are considered in the context of the patient’s condition, current phase of illness and in anticipation of deterioration.
This document will outline some of the key elements to consider when planning a discharge for a person with palliative and end of life care needs and will refer to useful resources that may be required for discharge.
NHS Fast Track for NHS Continuing Care
When a patient has a primary health care need arising from a rapidly deteriorating condition and an increased level of dependency, then they can be fast tracked for NHS Continuing Healthcare (a package of care or 24 hour nursing care home, arranged and funded by the NHS).
Completing the fast track assessment tool ensures that these individuals have continuing healthcare funding approved without delay, enabling them to be supported in their preferred place of care as quickly as possible without encountering any delays.
A referral to the hospital discharge planning team will be required to complete the necessary assessment and application for a fast track NHS continuing care funded discharge.
Rapid Discharge at the End of Life
This is a process to support the safe and timely discharge of patients who are thought to be actively dying in the last hours to days of life to their preferred place of death in the community. Part of this process typically involves applying for fast track NHS continuing healthcare funding, although the care may not be readily available at the point of discharge. In such an event, this should be clearly communicated to the patient where possible and to those closest to the patient.
A prompt referral to the hospital discharge planning team should be made as soon as it is determined that a patient requires a rapid discharge to die to their preferred place of death.
As rapid discharges are for patients recognised to be in the last hours or days of life, there is a risk that the patient may die whilst the discharge is being planned, during the transfer or shortly after arriving at their preferred destination. This risk should be clearly and sensitively communicated with the patient where possible and those closest to the patient, with a discussion on what would happen in that instance.
ReSPECT form
The Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) is a document that outlines personalised recommendations for a person’s goals of care and ceiling of treatment (including resuscitation) in a future emergency in which they are unable to make or express choices. It is created following discussions between the person and/or persons they’ve identified as important to them and their healthcare professionals.
It is valid in both hospital and community settings. If a patient is admitted to hospital with a ReSPECT form or uDNACPR form, a copy of this should be scanned in to HIVE and the original returned to the patient. Whilst in hospital a new version should be created in HIVE detailing the existing information and decisions, inclusive of any additional information or decisions made whilst an inpatient. At the point of discharge the ReSPECT form should be printed and this copy should then be signed by a doctor of an appropriate grade and discharged with the patient.
Statement of Intent
The aim of this document is to prevent the unnecessary attendance of the police in circumstances where a death has been anticipated (and does not need referral to coroner), but occurs at a time when the patient’s regular GP has not seen the patient in the last 14 days or is not immediately available to issue a Medical Certificate Cause of Death (MCCD).
If a patient is discharged home supported by the rapid discharge process, expected to die, and does not need referral to the coroner, the GP should review the patient as soon after discharge as possible to issue this.
A ‘bridging statement of intent’ can be issued in the meantime by an MFT doctor declaring they will be available as a medical practitioner to issue a medical certificate cause of death until such a time the GP has reviewed the patient and completed a Statement of intent. On occasions this may not be possible if there is not a medical practitioner available to issue the MCCD and therefore this should be highlighted to the patient’s community healthcare team including the GP prior to discharge to ensure a GP visit can be arranged as soon as possible.
TTO and Anticipatory Medications
Prior to discharging patients with longer term palliative care needs and those patients being supported with a fast track or rapid discharge at the end of life, it is important to review medications in the context of the persons condition and current phase of illness. Patients with palliative care needs should have their medications reviewed regularly to prevent polypharmacy and to ensure their medication regime remains appropriate for their needs. Any decision to modify or discontinue medications should be discussed where possible with the patient.
When a patient is recognised to be in the final hours or days of life it is important to review their medication regime and consider discontinuing non-essential medications and make plans for suitable alternatives for those medications considered essential, even when the oral route may no longer be reliable.
In addition to prescribing and supplying a patient’s regular regime of medications it is important to prescribe medications that may be required to treat any symptoms a patient may experience in the last hours – days of their life. They are given via the subcutaneous route and will need prescribing on the patient’s TTO. In addition to the supply of these medications, the direction to administer form should be completed to enable district nurses to administer them in the community setting.
These medications need to be prescribed on an individual basis following an appropriate assessment.
Patients requiring a syringe pump to support their symptom management should have these medications prescribed and supplied on their take home medication regime and the appropriate direction to administer form completed for the district nurses to be able to administer the infusion.
Prior to discharge, the syringe pump should be replenished to ensure the infusion does not run out before the district nurses are able to visit. When the district nurses visit the patient, they should replenish the syringe pump and change to a community device. Arrangements should be made to return the pump to the discharging hospital as per the local agreement.
Equipment
All patients with palliative care needs, and those having a rapid discharge home at the end of life should have equipment needed for discharge in place prior to discharge, unless otherwise discussed and agreed with the patient and those important to them; this may include practical equipment such as mobility aids, but may also include oxygen, suction machines and nebulisers.
Communication and Referrals
All patients with palliative care needs, and those having a rapid discharge home at the end of life should, with permission, be referred to the district nursing team; this supports the transition of care and ensures patients and those important to them are supported following a hospital admission.
All patients with palliative care needs, and those having a rapid discharge home at the end of life should have contact numbers for community teams they may need after discharge, particularly out of hours such as district nurses and GP. Ensure the patient and/or those important to them have these numbers.
All patients with palliative care needs, and those having a rapid discharge home at the end of life should have a discharge summary that reflects the events of the inpatient episode, their phase of illness, and any recommended follow up for the GP to note. If the patient is going home supported by a rapid discharge at the end of life, then the clinical team looking after the patient should phone the GP within working hours ahead of the discharge to ensure a visit can be planned as close to the discharge as possible.
Download the Palliative Care Discharge Policy [Word doc, 33KB]
In Manchester, we’ve a series of short term and long-term independent living options for people to call home for when they leave hospital or can no longer stay within their own home. These housing options for older people are Neighbourhood Apartments (short term temporary accommodation) and Extra Care Housing (long-term permanent accommodation) and are situated in the Integrated Neighbourhood Teams districts. Within this section, you can learn more about our independent living options and find out how you can apply and be linked to availability for Neighbourhood Apartments.
The District Nursing service delivers holistic quality assured nursing care to those aged 18 and over living in Manchester to ensure that patients and their carers are able to maximise their independence and to remain at home whenever possible.
There are slight variations in the way that charges are assessed in different care settings.
Non-Residential Care Services
When the charges are calculated, the council will make sure that payments do not leave a person with less than their Minimum Income Guarantee (MIG). The MIG is set each year by the Department of Health (DoH), and is the least amount of money a council must leave a person with after care charges (unless they are liable for the full cost of the care).
Residential Care Charges
Please consult your Local Authorities’ Charging Policies for more details.
For patients who live outside the Manchester and Trafford areas, early contact should be made with their relevant locality as soon as possible to plan discharge and make arrangements.
GM locality discharge contact details
| GM locality | Contact details | |||||||
| Bolton | Tel No: 01204 331 155 | |||||||
| Bury
|
0161 778 3078 (Mon-Fri)
0161 778 3481 (Mon-Fri) 0161 778 3582 (Weekends) You can download the Bury system admisison avoidance guide here- Bury – Final Admission Avoidance Alternatives 2023_24. |
|||||||
| Manchester | Tel No: 0161 2345 629
Email: control.room@manchester.gov.uk |
|||||||
| Oldham | Tel No: 0161 770 6771
Mobile: 07761405278 |
|||||||
| Rochdale | Tel No: 0300 303 8886 (Mon-Fri 8.30-4.45pm)
Tel No: 07976 308436 (Weekend and OOH) |
|||||||
| Salford | Tel No: 0161 206 4820 (Salford Royal IDT)
Tel No: 0161 206 0604 (Mon-Fri 8-6 pm) Tel No: 0161 206 4820 (Weekend and OOH) |
|||||||
| Stockport | Tel No: 0161 218 1730
Tel No: 0161 718 2118 (Weekend and OOH) Tel No: 0161 204 4644 (Crisis response) |
|||||||
| Tameside | Tel No: 0161 922 4888 (8.00 -6.00pm Mon –Fri)
Tel No: 0161 342 5656 (Weekend and OOH) Email: communitygateway@tgh.nhs.uk |
|||||||
| Trafford | Tel No: 0161 549 6912 | |||||||
| Wigan | Tel No: 01942 486911 | |||||||
| Blackburn | Tel: 01254 505 661
Tel: 01254 585 150 |
|||||||
| Lancashire | The contact for MLSCU is mlcsu.discharge2@nhs.net
Personalised Healthcare Commissioning Team Number 01772 952610 |
|||||||
Some people with long-term complex health needs qualify for free health and social care arranged and funded solely by the NHS. This is known as NHS continuing healthcare (CHC).
CHC supports people aged 18+ with long-term ongoing health needs from a disability, accident or illness. People who are eligible get a package of NHS-funded care that meets their care needs outside of hospital, for example in their own home or care home.
-
what help you need
-
how complex your needs are
-
how intense your needs can be
-
how unpredictable they are, including any risks to your health if the right care is not provided at the right time
If your needs change at any point, your eligibility for CHC may change too.
More information available on the GM Integrated Care Partnership website – NHS Continuing Healthcare
PTL Charter – Sept 2023 [PPT, 197KB]
Transfer of Care Hub [PPT, 90KB]
Glossary of Terms
Discharge to Assess (D2A)
An approach to intermediate care in which people are discharged from hospital as soon as medically ready so that long-term assessment can take place at or close to home instead of waiting to have that assessment while still in hospital.
Expected Discharge Date (EDD)
This is the date the patient leaves the hospital this should be moved as necessary to align with the clinical and discharge progress information. This should be recorded on HIVE
Criteria to Reside
Every person on every general ward should be reviewed on a twice-daily ward round to determine the following and recorded on HIVE. If the answer to each question is ‘no’, active consideration for discharge to a less acute setting must be made:
- requiring ITU or HDU care?
- requiring oxygen therapy/NIV?
- requiring intravenous fluids?
- NEWS2 greater than 3? (Clinical judgement required in persons with AF and/or chronic respiratory disease)
- diminished level of consciousness where recovery realistic?
- acute functional impairment in excess of home/community care provision?
- last hours of life?
- requiring intravenous medication > b.d. (including analgesia)?
- undergone lower limb surgery within 48 hours?
- undergone thorax-abdominal or pelvic surgery with 72 hours?
- within 24 hours of an invasive procedure? (With attendant risk of acute life- threatening deterioration)
Clinical exceptions will occur but must be warranted and justified. Recording the rationale will assist meaningful, time efficient review.
Strengths based approach.
A strengths-based approach focuses on an individuals’ strengths (including personal strengths and social and community networks) and not on their deficits. Strengths-based practice is holistic and multidisciplinary and works with the individual to promote their wellbeing.
It is an approach to working with a person that focuses on what they or their support network can do rather than approaching it from the perspective of what they cannot do.
Download Glossary of Terms [Word doc, 152KB]

Care Closer to Home – Urgent and Emergency Care Transformation Programme
The Manchester and Trafford system has come together to form a new programme of work to transform Urgent and Emergency Care (UEC). Care Closer to Home will involve four core programmes of work to improve outcomes for people on their journey from accessing urgent and emergency care right through to returning home with the right care in place to support their independence.
This involves working with community, social care and hospital services. The hospital-focused work will take place at the MRI with learning shared across MFT.
Alongside the work of system teams, we have commissioned an organisation called Newton Europe to provide additional support for this important programme.
What’s happened so far?
Work has been underway with colleagues across the system to scope the work, agree on priorities and plan for how we will make the improvements we want to see in UEC. The four programmes of work have been identified as:
- Right Patient Right Place
- Reducing Days Away from Home
- Short Term Services and Bedded Care
- System Vision and Active Leadership.
Care Closer to Home resources
You’ll find useful resources on Care Closer to Home in this section.
- Care Closer to Home Programme Charter [PDF 1.5MB] – sets out the programme aims and key work areas.